Laura Jenski
Topics:
The visual topic map is hidden for screen reader users. Please use the "Filter by Topic" dropdown menu or search box to find specific content in the transcript.
Doug Exton: Thank you so much for joining us for tonight's Connected Conversation, a program conducted by the Idaho Humanities Council. If you're not familiar with our organization, I encourage you to check out our website, Idaho Human .org. I'd also like to remind you all that you may submit any questions using the Q&A feature located at the bottom of the screen.
With me tonight is Laura Jenski, and it's a pleasure to have you with us tonight. And I turn it over to you.
Laura Jenski: Okay. Thank you. It's a pleasure to be here. Thanks for the opportunity. I'm going to go ahead and start my slides because it's. I was telling as I was saying, that I have a camera here. I have to look around at. Okay, there we go.
Okay. I would like to spend about 35 minutes telling you two stories and then, sharing some thoughts that I have about the current COVID vaccines. I will talk about smallpox because I think smallpox is just a wonderful illustration of of how a combination of luck and persistence can solve a problem that really seems unsolvable. And then I'll talk about polio, because polio is an example of how external influences external forces, outside of science, can affect vaccine development.
Let me say that my opinions are my opinions, they're not necessarily those of the Idaho Humanities Council. And also, I'm going to show you some, images of smallpox. And some people may find these images rather disturbing. So smallpox, the truly horrific disease, it's caused by the very old the virus, which is a DNA pox virus. And it starts with just simple flu like symptoms.
Then rash and then pus filled sores that scab over. So it really is a terrible disease to have, but it's a very old disease. It was past human to human, which means that there's no. And animal intermediate. There are no bats or rats or fleas or mosquitoes that will carry this very old virus. It has to be past human.
Human. So it probably didn't arise as a human condition until people started living in communities, like after the beginning of agricultural settlements, about, 10,000 B.C., you can find evidence of smallpox and mummified remains, like the Egyptian pharaoh, Ramses the Fifth. That would have been in, like, 1100 B.C.. But it really wasn't until the fourth century that you find written descriptions.
smallpox. Well, as I said, a horrific disease, very high mortality rate for smallpox, about 30%. And that's a rather misleading number because for the vulnerable, very old, the very young people with certain diseases, the mortality rate to be upwards of 90%. And even if you survived smallpox, you'd be, badly disfigured, especially on the face, because that's where you have the most, sebaceous glands that is oil producing glands.
And so that's where you get the most pockmarks. And in addition to the pox, the sores would sometimes get infected, and you'd have tissue damage, including tissue loss, like, you look at this picture of this poor woman in this photograph. She's lost part of her face, due to smallpox. Blindness was another problem. So, as you can well imagine, people, even though they didn't understand smallpox or didn't understand what it was, they were desperate for some relief from it.
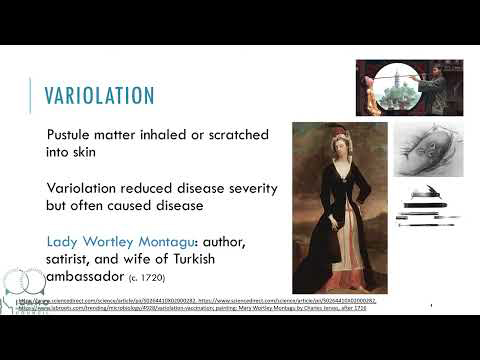
Well, over time, there evolved a method for some protection against smallpox. It's a method called inoculation, or more specifically, variolation. And that's a procedure where you take matter out of the pus filled sores, and you deliberately infect another person with the hope that they might get a real mild case of smallpox and then be prevented from getting a full blown case.
If you can see this slide in the upper corner. One method for variolation was to actually inhale the dried scabs off of people's skin. Another method that was practiced more in the Middle East and Africa was to take pus matter and scratch it into the skin using these pretty scary looking instruments. Here. And so, as awful as that sounds, very ablation actually didn't work to some degree and lessened disease severity.
But it also caused disease and sometimes it even caused deaths. One person that I want to talk about was who would have known about variolation, is a person called, Lady Mary Wortley Montagu. And she was the wife of the British ambassador to Turkey. Mary grew up in an aristocratic English family. She was apparently quite this free spirit.
She was a voracious reader. Read all the books in her family's library. And that gave her quite an education, which was unusual for a female at that time. This would have been the late 17th century. Well, in 1712, Mary eloped with Edward Wortley Montagu, against her father's wishes, and the newlyweds went to London. And Mary was a beautiful woman.
She was smart. So her beauty and her wit made her a fairly prominent feature. At the royal court. But sadly, about three years into her marriage, Lady Montagu contracted smallpox. Well, she survived, but she was disfigured. Her lovely face was badly marked. And on top of that, she had just two years earlier lost her favorite brother to smallpox.
So Lady Montagu was really passionate about finding some cure for this terrible disease. Well, when her husband was, assigned to Turkey and Lady Montagu followed him there, and that's where she learned about variolation. She would would see these elder Turkish women who would, in a ritual, use smallpox to attempt to prevent, full blown cases of smallpox.
So when Lady Montagu realized that they were going back to London, where smallpox was endemic, she had her five year old son variolated by the, embassy physician. And when she got back to London, she'd have her daughter variolated. And she did it very publicly. The same physician did the burial. Well, as you can imagine, the medical community didn't think very highly of that.
They didn't take variolation seriously. They thought it was some superstitious folk medicine. And of course, she was a woman. So they didn't take her seriously. But as I told you, she had some standing at court. And she had the ear of Caroline, the Princess of Wales, and she persuaded Caroline to ask her father in law, the King, to have the royal family variolated.
Well, the king agreed to test variolation. He had it tested on prisoners and orphans in asylum. Sounds bad. But the results were actually quite promising. It did reduce the mortality for Baryonyx for smallpox of down from 30% to 2 to 3%. So the king agreed that the females in the royal family, could be variolated.
He wasn't going to risk as male heirs. And that gave, some quite a bit credibility to variolation. And the medical establishment began to accept it. And throughout the 1700s, variolation became the the fairly common method to attempt to to protect against smallpox. But variation had risks. It wasn't regulated, and quite often it was combined with other pretty risky procedures like purges and bloodletting.
So, there were deaths. There were bad cases associated with the variolation, but still it was the only game in town. Throughout the 1700s. So enter Edward Jenner. Doctor Jenner was an English physician. He himself had been very ill fated. So he knew how awful the procedure could be. And he lived out in the country, which means he was aware that persons who had been exposed to a different pox disease, packs of cows very cleverly called cowpox.
He was aware that those persons didn't get smallpox. And the story goes that Doctor Jenner was so inspired by the beauty of the milkmaids faces that that he tested cowpox. Well, you know, that's probably not true, but Jenner was inspired to do scientific studies of cowpox. So what he did is he took, material from a cowpox lesion.
The milkmaid, Sarah Nelmes. Here's a drawing on the slide of the milkmaids hand. And he used that, pustular material to vaccinate, a young boy named James Phipps. If you're interested, this slide in the uppermost corner is what cowpox looks like on a cow. Anyway, so Jenner scratched the cowpox material into in under the skin of this young boy.
And then a few weeks later, he exposed the boy to small pox. And James didn't get smallpox. So Jenner exposed the smallpox again. And the boy didn't get smallpox then either. And, you know, you may be saying, oh, wait, wait a minute. How, it's totally unethical to be experimenting on children. Well, actually not really. That's at the time because, James would have been exposed to smallpox anyway.
Probably, as variolation, because there was, you know, an economic reason, to do so. So, again, that it was not considered unethical. Doctor Jenner is the person that gave us the term vaccination. He use the Latin word for cow, vacca. To coin that particular term. So that occurred this, work with the boy James Phipps occurred in 1796, and Jenner continued his experiments with other, let's call him volunteers.
And in 1798, Doctor Jenner published his work in a small booklet. Well, the medical community had sort of mixed reactions to his work. But Doctor Jenner was altruistic. He not only shared his knowledge, but he shared his cowpox vaccine. And over time, London physicians began to use this vaccination procedure themselves. And more and more of the medical community came on board with this idea that this using cowpox to protect against smallpox was safer and just as effective, if not more effective.
Society, on the other hand, had quite a bit of, shall we call it anti-vaccine sentiments? You can if you can see this cartoon in the slide here. These are, it's a cartoon of people who have been inoculated with, or vaccinated with cowpox, and they have cows popping out all over them. But over time, vaccination became more accepted.
Vaccination with cowpox was brought to America by the physician Benjamin Waterhouse. Doctor Waterhouse was a friend of Edward Jenner's. And, in 1800, when he brought vaccination to America, he received the endorsement of then President Thomas Jefferson. And that's actually remarkable, because Jefferson was known for being a harsh critic of, well, modern medicine for the time, modern for the time.
So when President Jefferson endorsed vaccination, there was more acceptance of it in the New World. And and America was already primed for this because variolation was already practiced here. Variolation. The use of smallpox to protect against smallpox was introduced to this country by African slaves. One of them in particular, Onesimus, shown here. Told the man who owned him, Cotton Mather, about that valuation and the benefits and the procedure.
Cotton Mather, you may recognize that name. That's the, Puritan minister who had some peripheral involvement in the Salem witch trials. Well, Mather publicized variolation widely. It was used by General Washington during the Revolutionary War because, I mean, Washington lost as many troops, if not more, to smallpox than in battle. By 1813, President Madison, enacted into law and, a law called an Act to Encourage Vaccination.
It created the United States Vaccine Agency, and it instructed the Postal Service to deliver the cowpox vaccine at no charge. So while this was happening in America, back in England, Edward Jenner died. He died in 1823 of a stroke. And at the time he died, he was about equally praised for his, enormous contribution to, vaccination and also vilified for his work.
About 17 years after his death, variolation, the actual use of smallpox, the the procedure that Lady Montagu had brought to England was banned in England in favor of vaccination. So let's fast forward and go into the 20th century. By the 1940s, the technology for freeze drying was perfected, and so the smallpox vaccine could be stored and distributed quite easily, and so could be, widely distributed worldwide, such that by 1980, the World Health Assembly had declared the world free of smallpox, and that was a magnificent accomplishment in, well, what seemed like very long time, but still, in terms of vaccine development, was only about 150 years.
Less than 200. Anyway. So, as you know, we are not routinely vaccinated for smallpox anymore. There still is a smallpox vaccine. It's held in a stockpile for high risk cases such as laboratory workers. It's, a vaccine, a virus. It's a live virus, attenuated, that is weakened. It's, not the same as. But it's related to smallpox and cowpox.
And it probably arose when the, smallpox and cowpox vaccines were, excuse me--viruses were passage in animals and humans in order to perpetuate materials to use as vaccines. And we have vaccines like this today. The Johnson Johnson vaccine and the AstraZeneca vaccine for COVID 19, are, live viruses. They are non virulent viruses, just like vaccine.
It's not a virus. And in the case of the COVID 19 viruses, they share some genetic material with the SARS COVID COV2 two virus. Just like that, Cynthia shares genetic material with the smallpox virus and is able to provide immunity against the smallpox. So I want to show you one more picture. This picture here on the right side of the screen.
These are two brothers photographed in the early 1900s. Boy on the right was vaccinated against smallpox. His brother on the left was not. And for me, if any image convinces me that vaccination is important. This image does it for me. So let's switch gears and talk about polio. I think we're probably more familiar with the disease polio than we are with smallpox.
Polio myelitis is a muscle weakness, and paralytic disease is caused by three state three strains of polio virus types one, two, and three. Type one is the most virulent strain, and it's another old disease. If you look back to Egyptian paintings, you know, 1300 1400 BC, you can see pictures of children with withered limbs that are using sticks like crutches.
But it wasn't until much later, 1789, that we actually got a clinical description of polio, described by an English physician. But polio was not a disease known for large outbreaks for most of its history. It wasn't really until the turn of the 20th century that polio virus became associated with outbreaks. And the reason for this is, up to this point, up until about 1900, polio virus was quite common in the environment.
Polio is, spread by the virus being, shed in fecal material, and then that contaminates the environment. And other people ingest the virus orally, and that spreads the disease, spreads the virus well up until the time that sanitation methods were vastly improved. Most infants would be exposed to polio virus in the environment while they were very young, and they still had antibodies from their mothers, in their bodies to protect them so they would be exposed to polio virus.
They would make an immune response and develop their own lifelong immunity to polio. At the time that antibodies was helping to protect them from getting a full blown paralytic disease. Well, once the sanitation procedures reduce the amount of polio virus in the environment, kids didn't get that early exposure to the polio virus, so they didn't make their own lifelong immunity while they still had.
antibodies to protect them. And so they became more susceptible to the virus. Well, the first major outbreak, I mean, as in very large outbreak of polio virus or poliomyelitis, was in 1916, in the United States, in New York, there were more than 27,000 reported cases of polio and 6000 deaths. Another important thing about this 1916 date is this heralded the beginning of the annual summer epidemics, outbreaks of polio.
Parents became quite worried about letting their children be out, among others, during the summer. They kept them out of public places, kept them out of public pools because they were very worried that their children would be, paralyzed for life. Now, I should mention that most, infections by the polio virus are asymptomatic, or they cause only mild flu like symptoms.
But 5% of the infections actually, go on to develop paralytic, paralysis or weakened muscles. So even though it was only a 5% chance, parents were still terrified at the prospect. So by 1952, we had our, largest outbreak of polio ever. There were more than 57 reported cases. And that's just the reported cases, 3000 deaths and more than 27,000 cases of paralysis.
So parents were terrified, and the cry for a polio vaccine was just absolutely deafening. Enter Jonas Salk and Albert Sabin. These were not the only polio. So they they weren't the first ones by any means, but they were the two scientists who brought effect of polio vaccines over the finish line. Doctor Salk at the University of Pittsburgh created a killed or inactivated virus vaccine.
And Albert Sabin at Cincinnati Children's Hospital created an attenuated or weakened vaccine, also known as the oral polio vaccine. So a little tidbit of information, if you're interested. The last, natural case of polio that originated in the US was in 1979.
So I like to talk about the race for a polio vaccine, because it so well illustrates how, forces outside of science can work on both the value and the limitations of science during vaccine development. So let's start the story in 1952. This again, this was the peak of a polio outbreak. So Jonas Salk, did a small clinical trial of his killed virus vaccine.
Institutionalize children. So these are children that are physically and mentally disabled. This is not how clinical trials are done today, but this was 1952. While the results were promising. The next year, Doctor Salk vaccinated himself and he vaccinated his family. The media covered all of this. And with all this media coverage, the, public began to expect that there was a polio vaccine, on the horizon.
So there was some pressure there. There were some scientists, I have to admit, that were, very critical of a killed vaccine. You have to remember, at this time, the vaccine were primarily attenuated or weakened viruses like the smallpox virus I just talked about or like the the, vaccines that were created by Louis Pasteur for rabies or for a couple, bacterial diseases, anthrax and chicken cholera.
Albert Sabin, in particular was critical. He said a killed vaccine was too risky. And then the fact that Jonas Salk used the most virulent form of the virus and his cold vaccine was even more problematic. Doctor Sabin said, you know, you should wait until an attenuated vaccine is available. Yeah, he worked on attenuated vaccines. You know, to be honest.
But, they didn't listen. And in 1954, there was a very large clinical trial controlled clinical trial of children where some children got to the kill vaccine and other children got, the placebo. Schools partnered with the clinical trial. So schools would send home consent forms to parents and the consent form made the parents ask to have their children in a clinical trial, rather than just simply give permission.
So it made participation in the trial, an honor, a civic duty.
It wasn't without some publicity problems. So? So the well known columnists, Walter Winchell, on one of his Sunday night radio broadcasts, claimed, miss claimed I should say that the that the vaccine had caused the deaths of monkeys and laboratory trials and the vaccines killer. But people listened to to Winchell and, that caused some of the parents to back off and say, I don't want my kid in in this clinical trial.
But public health experts pushed back on Winchell, and Jonas Salk also did. He called Walter Winchell, an armchair scientist, sidewalk superintendent. And that helped. That pushback helped, quite a number of parents then said, yes, let's enroll my child. And the clinical trial went forward starting April of 1954. Well, by 1955, they had some very encouraging results in media frenzy.
And the reports came out that the vaccine, the killed vaccine for polio, was 80 to 90% effective. So shortly thereafter, the vaccine was distributed widely and vaccinations began. And then the reports started trickling in, starting with a report by an Idaho physician who reported that, one of his patients had developed muscle weakness in the arm that had been vaccinated.
And and that's actually kind of unusual, because polio typically presents first as weakness in the legs. And then there were other reports, a total of 250 reports of vaccine induced polio and a total ten deaths. So, of course, vaccinations were halted and an investigation was started. And the investigation showed that all of the vaccine induced polio cases could be, localized to one manufacturer.
Cutter Labs in California. And apparently what happened was during the manufacturing process, the viruses had clumped, and the chemical formaldehyde that's used to kill virus couldn't get into the center of the clumps. And so there was still live virus there. And those who were vaccinated with that vaccine preparation were actually administered live virus. And they developed polio. Well, fortunately, that led to, much greater regulation and oversight of the manufacturing process.
And then ultimately, the vaccinations, resumed. Within about five years, the number of paralytic, polio cases were reduced from, more than 27,000 to about 2500, you know, about one tenth of that value. And the next year, in 1961, the FDA approved sabin's attenuated live polio virus or the oral oral polio vaccine. And the attenuated live virus, I believe is, is a better virus because it it better mimics the actual polio virus itself, the, disease causing virus.
And it causes a more robust immune response, particularly in the gut. So, as I was mentioning before, polio virus will replicate in the intestine and get shed in feces and it's that's the way it's spread into the environment for oral ingestion by others to become infected. So the attenuated vaccine would prevent the replication of the virus in the gut.
And so you wouldn't get the spread of the virus. Well, so the attenuated live vaccine is, is then the predominant vaccine in in the U.S. by 1968, the number of paralytic cases was much smaller than 100 a year. So very small number and the kill vaccine was phased out. But over time, there was renewed interest in and improved kill vaccine such that in 1997.
So, you know, only, nine years later, the improved kill vaccine was reinstated. And the reason for this interest in the kill vaccine is that in a very small number of cases, about one and 2.4 million vaccinations with the attenuated, vaccine, there would be there would occur a case of, vaccine induced polio. And usually in an immunocompromised person.
But 1 or 2.4 million is still not zero. So by the year 2000, the attenuated virus vaccine was, phased out in the United States, and the improved kill virus became the only vaccine for polio reduce in the in the U.S.. And this was fine because by this time the country had developed herd immunity. The, predominance of the virus, polio virus in the environment is very low, so the chances of an unimmunized person contracting the virus was diminishing was small.
But the, live attenuated vaccine is still used in other countries where polio is endemic. And because, as I said, it produces an immune response, a robust immune response helps prevent spread of the disease. It's cheaper to make, it's easier to distribute. And because it's an oral vaccine, you just take a drop, in the mouth or the Sugarcubes.
So it's very easy to administer. So you might be thinking, I'm going to end this with a rant about how, you shouldn't rush vaccine development to use the COVID vaccine development shouldn't be rushed. But that's absolutely not what I'm going to say, because I don't believe that at all. I don't believe that the current vaccines are rushed.
They are a new focus. The SARS-CoV-2 virus is a new VAX, a new virus for vaccine development. But the technology and scientific knowledge has been around for a long time. And I. I'd like to cherry pick just a few scientific discoveries to to try to support my argument. So let's start about 100 years ago. It was in the 1930s that antibodies were isolated in their proteins.
They were characterized, and they were found to be gamma globulins in the blood. So we've we've known a lot about antibodies for, almost 100 years. It's been about 70 years since we've known that, long term immunity is is the result of certain white blood cells called lymphocyte S, also called T and B cells. So we've we've known about the basis of long term immunity for a very long time as well.
Even the quote unquote modern term epitope has been around for, 60 years. So let me tell you what an epitope is. So if you can see this graphic of the corona of the COVID 19 virus, you've probably seen it way too often, you know, that, the surface of the virus, there is a protein called the spike or S protein.
And this, spike protein is how the virus interacts with the cell that it intends to infect. Well, the spike protein is a pretty big protein, and there are many parts to the protein and the the various parts are called epitopes. So this part of the molecule, this epitope here is interacting with the cell. The virus is known to infect.
So you can imagine if your body makes an antibody against this epitope that it will probably prevent infection. You will be a neutralizing antibody. Now will antibodies against some of these other epitopes be protective antibodies. Well we don't know. So it's important that vaccines have expressed in them the correct epitopes to give us protective immunity. But that's something we have known about for 60 plus years.
So it's really not, a novel concept. Well, some of the vaccines for COVID are, using mRNA technology. So let's talk about my RNA very briefly. MRNA, or messenger RNA, is the intermediary between our genes, which are made out of DNA, and our proteins, which carry out functions in our cells. So mRNA, it was officially discovered, in 1961, although, you know, it had been postulated to exist quite a number of years before that.
In 1986, the first vaccine, that that involved in nucleic acid DNA and RNA are both nucleic acids. The first FDA approved, DNA vaccine was, in existence, and it was a DNA vaccine for hepatitis. So even though that's a DNA, not an RNA vaccine, still, the concept of using nucleic acids as a vaccine is is a 35 year old.
I think that's the max 35. A year later, Crispr was discovered Crispr DNA sequences that are, used in a very elegant and and tailored genetic engineering that's possible today. And, you know, it was even 30 years ago. That's pretty a long time, maybe longer than some of you have been alive that, it was shown that you could inject mRNA into a living organism.
In this case, in 1990, it was a mouse. And show that the organism will make proteins. I encoded for by the mRNA. So that's the basis of the technology for the Moderna and the Pfizer vaccines right there in RNA vaccine. So it's been 30 years, that we've known that that particular method is possible. Also, these mRNA vaccines are, encapsulated in a fatty layer, called a lipid nanoparticle, shown here, in this slide.
Lipid nanoparticles have been around for 30 years as well. The first patent for them was filed in 1991. So I'd like to just end by saying that, we send my spiel by saying that, the reason I don't feel that the vaccines are being rushed, at least not that developed. The scientific development of the vaccine is because they are built on a very large and deep foundation of scientific knowledge and technology development.
So just to let you know, I get my layperson's information about COVID 19 vaccines from the New York Times. Coronavirus vaccine tracker. You can just Google it and find this website and, you can get a lot of information there. Now, I made these particular tables for myself, but this is the kind of information you could get at the website.
Who developed the vaccine once the vaccine made out of what's the status of it? Is it approved as it is for emergency use? Is it in clinical trials? And there is a lot of information there. If you are interested in in sort of going through. So I am going to end and let the conversation actually begin. If you would like to, contact me later with questions, I'm perfectly happy to have you do that.
You can email me at Laura Jen, ski at Snowbound stories.com, or you can go to my website, Snowbound stories.com. I have a contact form there and you know, you read about what I'm up to nowadays, which is writing mystery novels. So let me go ahead and end my slides and we'll see what kinds of questions we have.
Doug Exton: Thank you so much for all the information in there. I'm definitely not a science person, so a lot of that was really informative for me. You know, I heard about Jenner and smallpox vaccine, but that's kind of where my knowledge really stopped. One thing that I've heard a lot in the public sphere, you know, with comparisons with, you know, vaccines in general is, you know, the COVID 19 vaccine and the HIV Aids vaccine and how HIV doesn't have one yet.
However, there's been a lot of work towards that. So I was wondering if you, if you have the knowledge, if you're able to talk about that a little bit.
Laura Jenski: I'm, I'm actually not able to talk about that. I haven't, kept up with, the modern advances on the HIV vaccines.
Doug Exton: Yeah. I also, I do know that's a whole separate beast in its own right as the terms of the virus.
Laura Jenski: If it is, I will say that, you know, some of the basic technologies shared from one vaccine to another. It's the nature of the virus and what part of the virus you need to make an immune response at the ends that, requires the, the specialized tail ring, with. Which means that, you know, you really do have to focus on an individual virus to create the vaccine for.
And I'm sure that the HIV vaccine has a really interesting story. I just didn't, keep up with over the years.
Doug Exton: Well, you answered my next question, which was going to be, you know, what makes vaccines, you know, similar, but also kind of different, between each other. But what role does the public play in, you know, the production speed of a vaccine outside? Volunteering for clinical trial, you know, because some of those vaccines and the diseases you talked about had, you know, a really long period from, you know, start, I mean, obviously some of them were very old diseases, like you said, you know, to a vaccine compared to others.
Laura Jenski: So is the question, what can we do as private citizens.
Doug Exton: Yeah. Well not necessarily that. But you know, what do you think? What role can we play in terms of, you know, vaccine development? So actually I have to pretty much where you well.
Laura Jenski: I, I have I have a couple different answers. Choose the one you like. One of them is exactly what you were saying and that is participating in clinical trials. I don't know if you were paying attention to the numbers, but the, clinical trials for the various COVID vaccines were, in the tens of thousands of participants.
Compare that to, the, polio clinical trial in 1954, where there was well over a million participants. So clinical trials, because they're expensive, they they usually don't involve millions of people. But but you do need tens of thousands. So if you are able and willing, you should. You know, that's one thing you can do to help facilitate vaccine development.
And we need people of all ages, you know, usually vaccines are tested first on adults and then, you know, usually adults, perhaps up to the age of 55. And then they're tested on older adults and then they're tested on much younger people. So, yeah, participating, you know, and then there's money. You might want to let your, representatives know that they, they need to be supporting not only end phase development, where, you know, this is the last few steps before you start widely manufacturing, a vaccine.
I can tell you, that probably every scientific discovery that has had commercial value started out in some academic lab somewhere funded by the federal government, usually. And it would seem like such an esoteric thing to study. And, you know, the my, my favorite example, it's not a vaccine story, but it's still my favorite example. And and I'm sticking with it.
So in the 1960s, the scientists were injecting sinus glands, sinuses, glands right here, right over your heart. Sinus glands from, one strain a mouse into, another strain of mouse and vice versa. And then they were taking the antibodies out and testing the antibodies. And you you might stop and think, well, that is like the dumbest thing that actually spent federal money on.
But really, that was the start of our understanding of CD4 or and CD4, a positive T cells, which helped us then to understand Aids and and then help to combat Aids. So if that work with mice had not been funded in 1966, the work on Aids would have been set back. You know, a decade. I don't know if you remember.
Think Proxmire I think that's the name of the senator who used to give out the Golden Fleece Awards for, scientific studies that he thought were, not worthy. Well, you know, sometimes these esoteric studies are worthy. And so I would argue you need to make sure that basic science is supported, because that's going to be what vaccines eventually, use to for their final stages of development.
Doug Exton: And without that basic like fundamental building block, you really can't go further.
Laura Jenski: So if you don't understand this is true of anything, it's not just science, it's not just vaccines. If you don't understand the basics of a process, then you really can't. You can't troubleshoot, you can't improve it, and you may not even be able to conduct it. So, so yes, you you have to understand the basics. And it's particularly important in science when you're talking about something it's complicated as a vaccine.
Doug Exton: And would you consider the annual flu shot a vaccine. You know, since it is something you should be or, you know, have to do every year for that immunity?
Laura Jenski: Well, yes, it is a vaccine. There's very various formulations of it that's usually available. There are, killed virus vaccines for influenza. There are, there are some vaccines that have been engineered. So you just get, the important proteins from the virus, and the proteins are used as a vaccine. There's, at least there was last year.
Still a live attenuated vaccine. That was a nasal spray. So, I personally get a vaccine, every year for a flu. I've had flu once in my life. I never, ever want it again. I was like, in my early 40s at the time, and I was never, ever as sick as I was then. So flu shot, you know, easy.
Most insurance companies pay for it. They're safe. You maybe feel a little crummy for a little for a few hours, but, man, definitely worth it.
Doug Exton: And then, in your experience, in your research with the COVID 19 vaccine, there's been talk of, you know, a booster 12 months after your second dose. Do you think with that vaccine it could become, you know, something similar with the flu shot where you get a little booster every year?
Laura Jenski: I would not be at all surprised if that ends up being the regiment that's used. The early results tend to suggest that the mRNA vaccines are, long lasting. The immunity is long lasting. And we do know that attenuated virus vaccines like the Johnson Johnson vaccine should produce long term immunity. But, even well-established vaccines require booster.
Tetanus, rabies. These are all things that, occasion. And, I would not be surprised if we find that with the the creation of a number of variants, you know, if the COVID vaccine continues to remain in the population, if we don't reach herd immunity soon enough, we're going to have variants. And then the annual shots for annual boosters would help to combat the variants.
So I, I don't see any downside to it. Other than cost.
Doug Exton: And then speaking of variants, what happens when a virus or disease, you know, mutates in terms of vaccine production? Does it, you know, set it back by a decent amount or does it just kind of force you to, you know, shift, you know, your perspective of producing the vaccine?
Laura Jenski: Yeah. I, you know, and I think the influenza vaccines are an excellent example of how this is going to be handled. The influenza viruses mutate, readily so that every year you need a different, slightly different formulation. I don't think I would say that it's a setback in any way. I mean, it's it's just, a methodical process that, that scientists would go to to try to figure out the probability of what particular variant is going to be, most frequently found and to make sure that the vaccines protect you against that variant.
And, you know, in many cases, the the new viruses that arise will still have here's my favorite word, epitopes that, that you already have some immunity against. So you will already have some basal level of protection. You it's not like you have to start from ground zero. Every year.
Doug Exton: And then how has, you know, more like folk, traditional medicine and indigenous medical practices like, influenced either vaccines or treatment of these various diseases?
Laura Jenski: Well, unfortunately, the only one that pops right into my my mind is the one I've already talked about, and that is the this the history of smallpox. You know, I wish I had another example off the top of my head, but I don't. But it truly, it is the case that that over time, populations have found various remedies, available in nature, to health.
They may not be effective like, some of very well researched, very well manufactured vaccine might be, but they, they have been shown over time to have some effect. And that's an excellent question. You know, I I'm going to have to look that up. I'd like to know more about that. And I, I honestly don't.
Doug Exton: I always love stumping people with. Yeah. Well you're one question doing.
Laura Jenski: An excellent job tonight.
Doug Exton: Thank you. And then I know you talked about, you know, smallpox being completely eradicated. Well, you know, what happens, like, is there any true way to know, like, I don't want to be like, that paranoid person, but they're a true way to know that a virus has been completely eliminated, you know? And if it hasn't, how do you deal with that?
You know, sudden resurgence. If it does flare back up.
Laura Jenski: Okay. So. Well, of course it's not totally eliminated because we do have laboratory stockpiles of it. But that's not what you're asking. You're asking will it pop up again in nature? You know, that's not impossible. It arose once. So we know that the probability that it can arise is higher than zero. If it did arise, it the virus would have to find a human in order to infect it.
Because, as I said, there are no animal reservoirs for or vectors for this virus. For the smallpox virus. And so then what are the chances, you know, so we're doing some mathematics here. What are the chances that a very, infrequent mutation that creates this smallpox virus will actually also find human, that it can infect, and the human has no, resistance to it.
I think the probability of that happening will grow with time. As fewer and fewer people have any immunity to smallpox. Now, I was vaccinated against smallpox. I still have a scar on my arm to show where they scratched, the vaccinated virus into my skin. But, you know, after my generation, I don't know how many people have been vaccinated.
So at some point, there will be no, immune people. So if smallpox does arise, it's improbable as that might be, but it should a virus mutate and become the equivalent of a smallpox virus, and it finds a human to infect. Our best, remedy is that we do have these vaccines in a stockpile, and we could, tamp down the disease very quickly before it spreads throughout the population.
We know that it spreads pretty quickly. And we would also know how to make the virus pretty quickly using modern technology.
Doug Exton: And it's one thing that I always find super interesting in this, you know, again, could just be the way that I pay attention to media and also the way the media reports on it. But I always feel like with a lot of these different diseases that can be fatal, it seems like there's random flare ups that happen, and then it just kind of goes, you know, back to being quiet for a little bit.
Like with Ebola, you know, and and again, like I said, I could just be the way I've seen it portrayed in the media as like, oh, it's a random flare up, you know, here. And then it just kind of dies down a little bit. Is that, you know, an accurate representation of how some of these viruses that are still around kind of act like act in a way.
Laura Jenski: And you bring up an excellent example when you talk about like the first SARS outbreak in the Mas, outbreak, which is a related virus. Those are viruses. It's a it's a type of virus that actually will live in animals. So you have a reservoir and it doesn't have to be spread person to person. You the virus can live in an animal.
And then,
It's some if all the stars aligned and the, the animal is shedding the virus in a place where a person can pick it up and that person has no immunity, then you know, it kind of sets the stage for, an outbreak. It's if there isn't an animal reservoir for a particular disease causing organisms, then once you eradicated from humans, you would expect that it's gone until you have some almost improbable mutation event to make it reappear.
Doug Exton: Thank you for all of your answers. Unfortunately, we are out of time tonight. I will definitely be posting your contact, email when we post the recording of this. That way people can reach out to you for further questions. And one thing I definitely want to commend is, you know, like I said earlier, I'm not a science guy, and I definitely think you explained everything in like the most understandable way because I think, you know, learning about vaccines can definitely be one of those intimidating topics.
Laura Jenski: Well, I have to admit, it is one of my favorite subjects and I can get pretty excited about it. But but thank you. Thank you for the opportunity to do this. This is a lot of fun and I really enjoy it. So. And I have a good evening.
Doug Exton: Yeah. You too. Have a good evening, everyone.